Overall, we estimate that, while 83% to 88% of the population may become infected, most people are expected to have no or mild symptoms
Overall, we estimate that, while 83% to 88% of the population may become infected, most people are expected to have no or mild symptoms
Models are tools that can help you think about the future. But they don’t tell you the future in the sense that someone with a crystal ball might tell you the future.
On Wednesday, we released two reports on behalf of the South African Covid-19 Modelling Consortium.
The reports provide projections for the spread of the epidemic at the national and provincial levels.
Like all models, the National Covid-19 Epi Model, which generates the projections, comprises a set of formal assumptions about how the world might work. This article is intended to shed light on some of those assumptions, as well as explain major sources of uncertainty and discuss some limitations and next steps.
Developing a mathematical model to simulate the spread of a disease in the context of public health is a multidisciplinary and collaborative process.
It would be incorrect to assume that a disease model applied to different settings or countries would result in the same findings.
Though the biological assumptions on disease transmission may be the similar across settings, there are vast differences to be accounted for in health infrastructure, national health management policy, methods of prevention, operational challenges, population behaviour and access to care.
It is therefore important to work with disease and public health specialists to collate available information for the model before transforming this data into equations, algorithms and computer code.
And as no two countries, health systems and populations are the same, so too, will each disease model be unique and have its own challenges.
Current estimates
Let’s review the numbers.
The current version of the model estimates that South Africa can expect a total of 12 million to 13 million symptomatic cases of Covid-19 to have accumulated by early November.
The epidemic may peak, with around 1 million active cases, between mid-July and late August.
Overall, we estimate that, while 83% to 88% of the population may become infected, most people are expected to have no or mild symptoms.
Only about 1% of the population is expected to develop severe symptoms; however, we expect that this 1% will be sick enough to need hospitalisation.
As a result, the projections suggest that hospital capacity is likely to be overwhelmed, with all ICU beds, in the public and private sector, filled by mid-July, or earlier.
There are, however, many factors that could cause deviations from these projections, including individual behavior change and tighter (or looser) restrictions than we currently assume.
The modelling approach
The projections are generated using a type of model that represents the population as a number of mutually exclusive groups, commonly known as “compartments”.
These groups represent different infection and disease states.
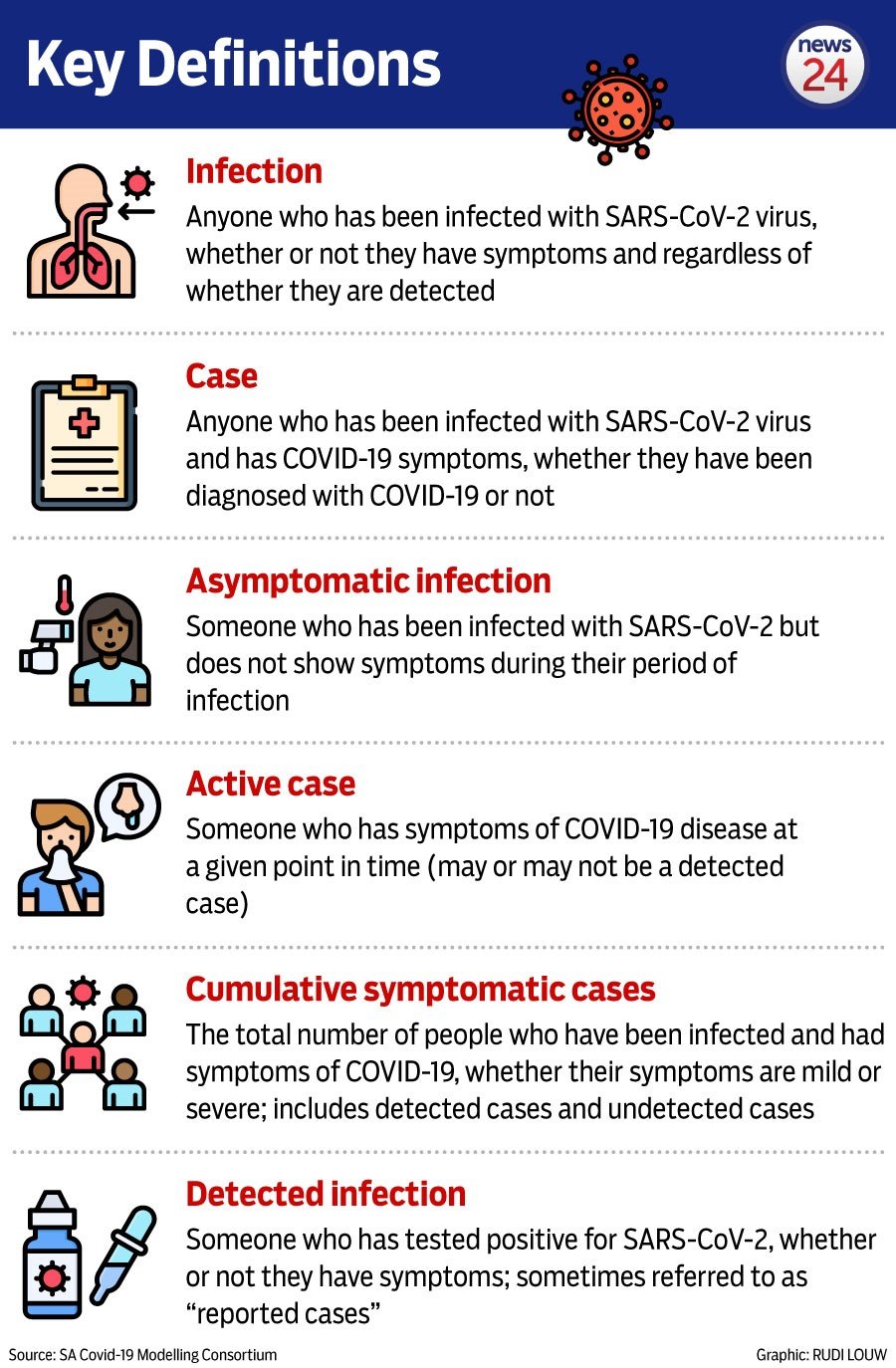
In the National Covid-19 Epi Model, there are compartments representing susceptible people, those who have been infected but are not yet able to transmit the virus, those who are infectious but not ill (either asymptomatic or presymptomatic), multiple groups of ill individuals (e.g., those with mild or severe illness, those in hospital, and those in ICU), recovered people, and those who have died.
Each of the compartments is tracked through time, and the number of new infections depends on the interaction between the numbers of susceptible and infectious people.
The model also keeps track of how and when people in different compartments get tested, which allows us to project the number of cases that will be detected by particular dates.
In order to run the model, we have to set values for the rates and probabilities of people transitioning between the various compartments.
Deciding on which values to use has been an important role of the broader South African Covid-19 Modelling Consortium.
The Consortium is a group of researchers from academic, non-profit, and government institutions across South Africa who work to provide, assess, and validate model projections for government planning purposes.
The group includes not just modellers, but also epidemiologists, virologists, actuaries, intensivists and other clinicians, and demographers.
These experts from diverse fields have given extensive input based on their own experience and on their knowledge of the global literature to inform the values used in the models.
Nevertheless, there are some values that can’t be estimated directly from data or based on existing expertise.
For example, the model allows us to modify the transmission rate by adjusting the rate of contact between individuals in the population through time, but it is particularly difficult to determine values for the transmission rate in relation to the efficacy of intervention measures.
For this reason, we have considered two different scenarios when looking at the long-term projections.
Under the optimistic scenario, we assume that the Level 5 lockdown reduced the contact rate by 60%, the Level 4 lockdown reduced the contact rate by 35%, and measures in place after 31 May will reduce the contact rate by 20%, relative to pre-lockdown levels (what we used to know as “normal life”).
Under the pessimistic scenario, we assume that the Level 5 lockdown reduced the contact rate by only 40%, Level 4 reduces the contact rate by 25%, and measures in place after 31 May will reduce the contact rate by 10%.
The projections vary under the two scenarios.
Key assumptions
No country knows the true number of people infected with Covid-19. The number of laboratory-confirmed cases depend on the testing criteria and testing capacity of the country.
As has been the experience of many countries around the world, the majority of Covid-19 infections will show no or only mild symptoms, with only a fraction of those seeking care at outpatient or hospital facilities or Covid-19 testing.
Therefore, the true total number of people infected with Covid-19 (which is what our total infection projections show) is much higher than the number of cases reported.
We focus on these numbers however, as we will believe that severe cases will present for hospitalisation and require care regardless of whether or not they have been tested and identified as Covid-19 positive.
Important uncertainties
Disease models help us understand and unpack the key drivers of infection, the many uncertainties and the likely impact of interventions.
As Covid-19 is a new infectious disease, there are still many things that are unknown.
Some of these unknowns are about the disease generally (e.g. how many people who are infected never develop symptoms, how long does immunity last after infection) and some are specific to South Africa (e.g. how does South Africa’s disease and age profile influence the severity of Covid-19 infections?).
We don’t know whether people living with HIV and/or TB are more susceptible to infection, or whether they experience more severe disease. There is also very little evidence on the role of children in transmission.
There is considerable uncertainty regarding the proportion of infected individuals who remain asymptomatic, and the relative infectiousness and the duration of infectiousness of these asymptomatic individuals.
This has important implications for the transmission dynamics in the model and the projected number of hospitalisations and deaths. One way that scientists explore the impacts of uncertainty is to conduct what’s known as a “sensitivity analysis” – essentially asking the question of how sensitive key results are to the assumptions that are made in areas of uncertainty.
Our national long-term report contains an example of a sensitivity analysis focused on understanding the importance of the assumptions made about asymptomatic infections.
We run multiple scenarios to help us understand how the epidemic may progress under different assumptions and uncertainties.
This enables us to explore which of the unknowns will have a big impact on the trajectory of the epidemic. Our projections show a probable range of values rather than a single estimate, which capture some of this uncertainty.
What are the next steps?
We are continuously updating our model as new data become available. This includes re-calibrating the model to match observed trends of detected cases and deaths in South Africa.
We also keep abreast of the global scientific literature and adjust our underlying assumptions when new information becomes available.
For example, earlier versions of the model assumed that most infections would cause symptomatic cases; however, new data and analyses suggest that the asymptomatic proportion of infections is higher, so we have adjusted the corresponding value in the model.
We are also in the process of adapting the model to better represent the patterns of hospitalisation times and outcomes to reflect data from South Africa.
The model also changes when new questions get asked. Currently, we’re developing new versions of the model that will account for the excess mortality expected once the country’s health care capacity is breached, and that will allow us to more flexibly investigate a range of interventions, particularly ones that focus on reducing contact for specific age groups.
We also continually improve our model based on ongoing peer-review. This makes the model projections more reliable over time.
In conclusion
As we said at the beginning, models are tools that can help us think about the future. They do not tell us what the future will hold. The projections we have made are based on a simplified, and fairly pessimistic, set of assumptions about people’s behaviour.
The true outcome of the epidemic will depend on many factors, and one of the most important factors will be individuals’ behaviour.
We can each of us help continue to flatten the curve by reducing our contacts, observing physical distancing, washing our hands well and often, wearing non-medical masks, isolating ourselves when we are sick, and quarantining ourselves when we know we’ve been in contact with someone who was infected.
Changing the course of the epidemic is our shared responsibility.
About the authors:
Prof. Juliet Pulliam is the Director of the South African Centre for Epidemiological Modelling and Analysis (SACEMA), which is a national DSI-NRF Centre of Excellence hosted by Stellenbosch University. She is also a Professor of Applied Mathematics at Stellenbosch University. Prior to moving to SACEMA in July 2016, she spent five years as a faculty member in the Department of Biology and the Emerging Pathogens Institute (EPI) at the University of Florida. Juliet received a PhD in Ecology and Evolutionary Biology from Princeton University in 2007 and spent three years as a Research and Policy for Infectious Disease Dynamics (RAPIDD) Program Fellow at the US National Institute of Health’s Fogarty International Center. Her research focuses on applications of mathematical modelling to applied questions in infectious disease epidemiology, with a particular focus on emerging, zoonotic, and vector-borne pathogens.
Dr Sheetal Silal is the Director of the Modelling and Simulation Hub, Africa (MASHA) and senior lecturer in the Department of Statistical Sciences at the University of Cape Town (UCT). She is an Honorary Visiting Research Fellow in Tropical Disease Modelling at the Nuffield Department of Medicine at Oxford University. She received a PhD in Mathematical Modelling of Infectious Diseases in 2014 from UCT. Her primary research area is the development and application of mathematical models to malaria, pertussis, and other infectious diseases in South Africa, sub-Saharan Africa and globally, with a focus on using mathematical models to predict the dynamics and control of diseases to evaluate the potential impact of control programmes in reducing morbidity and mortality, and supporting policy development.
Gesine Meyer-Rath, MD, PhD, is a medical doctor and health economist working on the economics of infectious disease interventions in low- and middle-income settings. She is an Associate Professor at the Center for Global Health and Development, Boston University, US, and lives in Johannesburg where she works at the Health Economics and Epidemiology Research Office (HE2RO), a collaboration between Boston University and the University of the Witwatersrand. Her focus lies on modeling methods for economic evaluation and translating research into recommendations for public policy.
Dr Harry Moultrie is a medical doctor and epidemiologist at the NICD’s Centre for Tuberculosis. His current research focus is the geospatial distribution of TB in South Africa. He has worked on a number of peer-reviewed journal articles on, among others, antiretroviral therapy and HIV/AIDS.